Introduction: Primary central nervous lymphoma (PCNSL) is a rare type of non-Hodgkin lymphoma that may involve the brain, spinal cord, leptomeninges and vitreous. The median age at diagnosis is in the fifth decade and most patients (pts) present with significant neurologic deficit and a low performance status. The optimal treatment of PCNSL is controversial. High dose methotrexate (HDMTX) is a standard treatment of PCNSL and is more effective when given in combination with other CNS-penetrating medications, which, however, add to the toxicity of the treatment. We aimed to evaluate the effectiveness and the safety of the combination of rituximab, HDMTX, procarbazine and lomustine (R-MPL) in pts with PCNSL.
Patients and methods: We retrospectively reviewed the files of PCNSL pts treated in Hadassah Medical Center, Jerusalem, Israel, between the years 2006-2019. The medical records were reviewed for demographic details and initial disease characteristics (age, sex, performance status, laboratory results, cerebrospinal fluid (CSF) content and tumor location), and for therapeutic details including chemotherapy protocol, toxicity, response to treatment and survival. We excluded pts who could not receive HDMTX.
The R-MPL is a 42-day cycle protocol, consisting IV Rituximab 375 mg/m2 on days 1, 15 and 28, IV HDMTX 5 g/m2 (3.5 g/m2 for pts > 60 Years (y)) on days 2, 15 and 29, PO procarbazine 100 mg/m2 (60 mg/m2 for pts > 60 y) on days 3-9, PO lomustine 60 mg/m2 (40 mg/m2 for pts > 60 y) on day 2. Six to nine intrathecal (IT) injections of MTX / cytarabine were included for pts with positive CSF cytology, tumor adjacent to ventricles, or per physician's decision. Rituximab was given for no more than 8 doses in total. A total of 3-4 courses of R-MPL were given. Responsive pts could proceed to autologous stem cell transplant (ASCT) with TECAM conditioning or 2 cycles of intermediate dose cytarabine (IDAC, 1.5 g/m2), 2 doses in each cycle. Those who achieved less than CR or had significant toxicity to R-MPL received additional ifosfamide/etoposide or high dose cytarabine or temazolamide or topotecan. Radiation was given only for salvage.
Results: Fifty-two pts were included in the study. Median age was 62 years (range 28-94). Three (6%) had leptomeningeal involvement, thirteen (25%) had vitreoretinal involvement, 30 (58%) had involvement of the deep brain. Mean ECOG, IELSG and MSKCC scores were 1.98, 2.53 and 1.94 respectively. The median number of HDMTX doses was 8 (range 3-16). Forty-five (87%) pts completed at least one 42-day cycle of R-MPL. Among this group, 29 (64%) pts received at least 3 IT injections, 12 (27%) underwent ASCT, 10 (22%) received IDAC, and 7 (16%) received other chemotherapies. The median follow-up was 27 months (m) (range 0.4-140m).
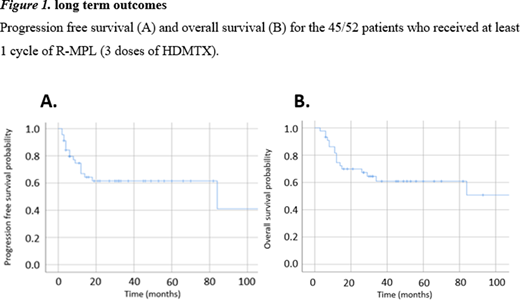
The overall response rate (ORR) was 79% (41/52), and the complete response (CR) rate was 52% (27/52). The median progression free survival (PFS) was 15.5m and the median overall survival (OS) was 27m. Among the 45 pts who received at least one R-MPL cycle, the ORR was 87% (39/45), the CR rate was 60% (27/45), the median PFS was 84m and the median OS was not reached (figure 1).
Known prognostic factors correlated with OS: age (p<0.01), ECOG performance status (p<0.01), CSF protein (p=0.01) and IELSG/MSKCC scores (p=0.05/0.04). Patients who received at least 3 IT injections had a trend to longer PFS (32.4m Vs 19.2m, p=0.09), and a significant OS benefit (48.6m Vs 20.8m, p<0.01). In a multivariable model, the effect of IT injections was independent of age, sex and IELSG score, and attenuated by number of HDMTX doses.
ASCT/IDAC did not improve PFS/OS, however numbers were small. Achieving CR at the end of treatment strongly correlated with PFS/OS, but timing of best response (after one 42-day cycle Vs later) did not.
Grade 3-4 adverse events included infections (21%) and kidney injury (13%). Two pts died during therapy, both in the 1st cycle due to disease progression. Ten pts (19%) discontinued therapy due to toxicity. No treatment related mortality (TRM) was documented.
Conclusions: The R-MPL protocol achieved a favorable ORR/PFS/OS as described, with reasonable grade 3-4 toxicity and no TRM. The advantage of ASCT/IDAC could not be assessed due to small number of pts. IT injections (at least 3) and achievement of CR at the end of treatment correlated with survival. The R-MPL protocol was reported in previous trials only among the elderly, and should further be evaluated in all age groups.
Goldschmidt:Abbvie Inc: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal